Reposicionamiento de Fármacos: Nuevos Caminos para Medicamentos Conocidos
DOI:
https://doi.org/10.18633/biotecnia.v27.2591Palabras clave:
Reposicionamiento, antiinflamatorio no esteroideo, sildenafil, omeprazol, bioinformáticaResumen
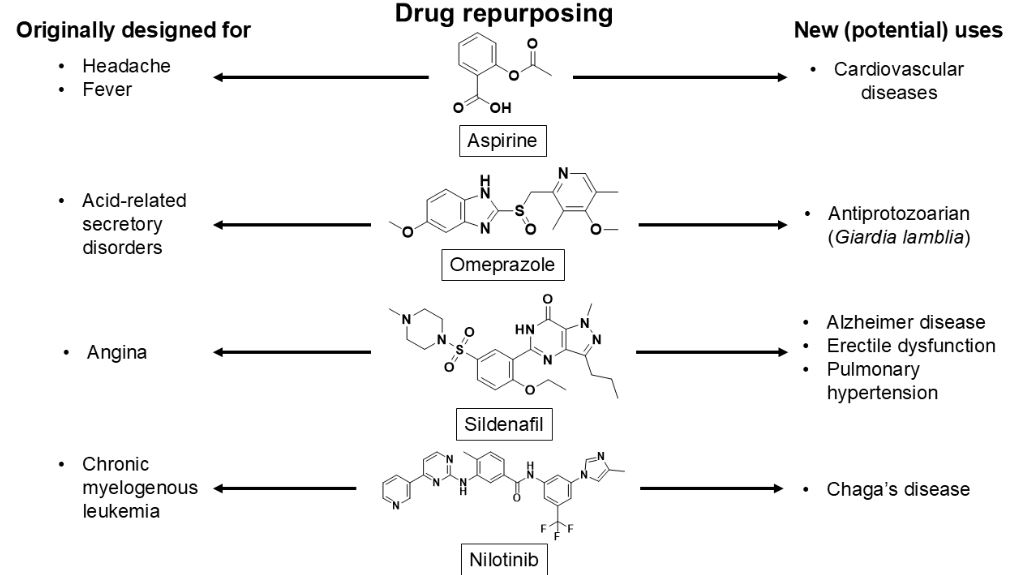
El reposicionamiento de fármacos es una estrategia que aprovecha medicamentos aprobados para tratar enfermedades distintas a las originalmente previstas. Este enfoque reduce tiempo y costos asociados al desarrollo de nuevos fármacos, facilitando el descubrimiento de nuevas opciones terapéuticas. Esta revisión tiene como objetivo explorar las metodologías utilizadas, los desafíos actuales y el impacto potencial de este enfoque en la medicina. Se realizó una búsqueda en las bases de datos PubMed y ScienceDirect utilizando palabras clave relacionadas con el reposiciona[1]miento de fármacos, combinando términos como “repurposing” con diferentes tipos de medicamentos. Se priorizó la información más reciente, específicamente de los últimos 15 años (tomando 2010 como límite), y se excluyeron artículos irrelevantes o desactualizados. Se destacan casos exitosos de reposicionamiento, como el ibuprofeno, un antiinflamatorio no esteroideo (AINE) estudiado contra enfermedades neurodegenerativas. El ácido acetilsalicílico, diseñado inicialmente para la hipertensión y angina, que ha mostrado actividad contra el cáncer y Alzheimer; y el omeprazol, utilizado para la gastritis, ha demostrado actividad antiparasitaria. Estos ejemplos subrayan cómo fármacos aprobados, con perfiles de seguridad establecidos, pueden tener nuevos usos. El reposicionamiento de fármacos, apoyado por herramientas bioinformáticas, representa una vía prometedora para tratar enfermedades desatendidas y mejorar terapias mediante combinaciones que optimizan la eficacia y reducen efectos secundarios.
Descargas
Citas
Amano, Y., Namatame, I., Tateishi, Y., Honboh, K., Tanabe, E., Niimi, T., & Sakashita, H. (2015). Structural insights into the novel inhibition mechanism of Trypanosoma cruzi spermidine synthase. Acta Crystallographica. Section D, Biological Crystallography, 71(Pt 9), 1879–1889.
Borba-Santos, L. P., Nucci, M., Ferreira-Pereira, A., & Rozental, S. (2021). Anti-Sporothrix activity of ibuprofen combined with antifungal. Brazilian Journal of Microbiology, 52(1), 101.
Chan, A. T., Giovannucci, E. L., Meyerhardt, J. A., Schernhammer, E. S., Curhan, G. C., & Fuchs, C. S. (2005). Long-term use of aspirin and nonsteroidal anti-inflammatory drugs and risk of colorectal cancer. JAMA, 294(8), 914–923.
Chan, A. T., Giovannucci, E. L., Meyerhardt, J. A., Schernhammer, E. S., Wu, K., & Fuchs, C. S. (2008). Aspirin dose and duration of use and risk of colorectal cancer in men. Gastroenterology, 134(1), 21–28.
Chan, A. T., Ogino, S., & Fuchs, C. S. (2007). Aspirin and the risk of colorectal cancer in relation to the expression of COX-2. The New England Journal of Medicine, 356(21), 2131–2142.
Chen, L., Liu, Y., Becher, A., DIepold, K., Schmid, E., Fehn, A., Brunner, C., Rouhi, A., Chiosis, G., Cronauer, M., Seufferlein, T., & Azoitei, N. (2020). Sildenafil triggers tumor lethality through altered expression of HSP90 and degradation of PKD2. Carcinogenesis, 41(10), 1421–1431.
Cofer, L. B., Barrett, T. J., & Berger, J. S. (2022). Aspirin for the Primary Prevention of Cardio-vascular Disease: Time for a Platelet-Guided Approach. Arteriosclerosis, Thrombosis, and Vascular Biology, 42(10), 1207–1216.
Das, A., Durrant, D., Mitchell, C., Mayton, E., Hoke, N. N., Salloum, F. N., Park, M. A., Qureshi, I., Lee, R., Dent, P., & Kukreja, R. C. (2010). Sildenafil increases chemotherapeutic efficacy of dox-orubicin in prostate cancer and ameliorates cardiac dysfunction. Proceedings of the National Academy of Sciences of the United States of America, 107(42), 18202–18207.
Fijałkowski, Ł., Skubiszewska, M., Grześk, G., Koech, F. K., & Nowaczyk, A. (2022). Acetylsali-cylic Acid–Primus Inter Pares in Pharmacology. Molecules 2022, Vol. 27, Page 8412, 27(23), 8412.
García-Torres, I., De La Mora-De La Mora, I., Marcial-Quino, J., Gómez-Manzo, S., Vanoye-Carlo, A., Navarrete-Vázquez, G., Colín-Lozano, B., Gutiérrez-Castrellón, P., Sierra-Palacios, E., Ló-pez-Velázquez, G., & Enríquez-Flores, S. (2016). Proton pump inhibitors drastically modify tri-osephosphate isomerase from Giardia lamblia at functional and structural levels, providing molecular leads in the design of new antigiardiasic drugs. Biochimica et Biophysica Acta, 1860(1 Pt A), 97–107.
Ghofrani, H. A., Osterloh, I. H., & Grimminger, F. (2006). Sildenafil: from angina to erectile dys-function to pulmonary hypertension and beyond. Nature Reviews. Drug Discovery, 5(8), 689.
Gohel, D., Zhang, P., Gupta, A. K., Li, Y., Chiang, C. W., Li, L., Hou, Y., Pieper, A. A., Cummings, J., & Cheng, F. (2024). Sildenafil as a Candidate Drug for Alzheimer’s Disease: Real-World Patient Data Observation and Mechanistic Observations from Patient-Induced Pluripotent Stem Cell-Derived Neurons. Journal of Alzheimer’s Disease : JAD, 98(2), 643–657.
Guo, C. G., Ma, W., Drew, D. A., Cao, Y., Nguyen, L. H., Joshi, A. D., Ng, K., Ogino, S., Mey-erhardt, J. A., Song, M., Leung, W. K., Giovannucci, E. L., & Chan, A. T. (2021). Aspirin Use and Risk of Colorectal Cancer Among Older Adults. JAMA Oncology, 7(3), 1.
Hersh, E. V., Hammond, B. F., & Fleury, A. A. P. (1991). Antimicrobial activity of flurbiprofen and ibuprofen in vitro against six common periodontal pathogens. The Journal of Clinical Dentistry, 3(1), 1–5.
Juárez-Saldivar, A., Schroeder, M., Salentin, S., Joachim Haupt, V., Saavedra, E., Vázquez, C., Reyes-Espinosa, F., Herrera-Mayorga, V., Villalobos-Rocha, J. C., García-Pérez, C. A., Campillo, N. E., & Rivera, G. (2020). Computational Drug Repositioning for Chagas Disease Using Pro-tein-Ligand Interaction Profiling. International Journal of Molecular Sciences 2020, Vol. 21, Page 4270, 21(12), 4270.
Kaur, D., Choudhury, C., Yadav, R., Kumari, L., & Bhatia, A. (2024). Aspirin as a potential drug repurposing candidate targeting estrogen receptor alpha in breast cancer: a molecular dynamics and in-vitro study. Journal of Biomolecular Structure and Dynamics.
Konstan, M. W., Byard, P. J., Hoppel, C. L., & Davis, P. B. (1995). Effect of High-Dose Ibuprofen in Patients with Cystic Fibrosis. New England Journal of Medicine, 332(13), 848–854.
Lands, L. C., & Dauletbaev, N. (2010). High-Dose Ibuprofen in Cystic Fibrosis. Pharmaceuticals, 3(7), 2213.
Lands, L. C., & Stanojevic, S. (2019). Oral non-steroidal anti-inflammatory drug therapy for lung disease in cystic fibrosis. Cochrane Database of Systematic Reviews, 2019(9).
Patrono, C., & Rocca, B. (2021). Aspirin at 120: Retiring, recombining, or repurposing? Research and Practice in Thrombosis and Haemostasis, 5(4).
Pérez-Villanueva, J., Romo-Mancillas, A., Hernández-Campos, A., Yépez-Mulia, L., Hernán-dez-Luis, F., & Castillo, R. (2011). Antiprotozoal activity of proton-pump inhibitors. Bioorganic & Medicinal Chemistry Letters, 21(24), 7351–7354.
Pina-Vaz, C., Sansonetty, F., Rodrigues, A. G., Martinez-De-Oliveira, J., Fonseca, A. F., & Mardh, P. A. (2000). Antifungal activity of ibuprofen alone and in combination with fluconazole against Candida species. Journal of Medical Microbiology, 49(9), 831–840.
Planer, J. D., Hulverson, M. A., Arif, J. A., Ranade, R. M., Don, R., & Buckner, F. S. (2014). Synergy Testing of FDA-Approved Drugs Identifies Potent Drug Combinations against Trypano-soma cruzi. PLOS Neglected Tropical Diseases, 8(7), e2977.
Reigada, C., Valera-Vera, E. A., Sayé, M., Errasti, A. E., Avila, C. C., Miranda, M. R., & Pereira, C. A. (2017). Trypanocidal Effect of Isotretinoin through the Inhibition of Polyamine and Amino Acid Transporters in Trypanosoma cruzi. PLOS Neglected Tropical Diseases, 11(3), e0005472.
Reyes-Vivas, H., De La Mora-De La Mora, I., Castillo-Villanueva, A., Yépez-Mulia, L., Hernán-dez-Alcántara, G., Figueroa-Salazar, R., García-Torres, I., Gómez-Manzo, S., Méndez, S. T., Va-noye-Carlo, A., Marcial-Quino, J., Torres-Arroyo, A., Oria-Hernández, J., Gutiérrez-Castrellón, P., Enríquez-Flores, S., & López-Velázquez, G. (2014). Giardial Triosephosphate Isomerase as Possible Target of the Cytotoxic Effect of Omeprazole in Giardia lamblia. Antimicrobial Agents and Chemotherapy, 58(12), 7072.
Rial, M. S., Reigada, C., Prado, N., Bua, J., Esteva, M., Pereira, C. A., & Fichera, L. E. (2023). Effectiveness of the repurposed drug isotretinoin in an experimental murine model of Chagas dis-ease. Acta Tropica, 242.
Sanyal, A. K., Roy, D., Chowdhury, B., & Banerjee, A. B. (1993). Ibuprofen, a unique anti‐inflammatory compound with antifungal activity against dermatophytes. Letters in Applied Micro-biology, 17(3), 109–111.
Shah, P. N., Marshall-Batty, K. R., Smolen, J. A., Tagaev, J. A., Chen, Q., Rodesney, C. A., Le, H. H., Gordon, V. D., Greenberg, D. E., & Cannon, C. L. (2018). Antimicrobial Activity of Ibuprofen against Cystic Fibrosis-Associated Gram-Negative Pathogens. Antimicrobial Agents and Chemo-therapy, 62(3).
Sobhani, K., Li, J., & Cortes, M. (2023). Nonsteroidal Anti-Inflammatory Drugs (NSAIDs). First Aid Perioperative Ultrasound: Acute Pain Manual for Surgical Procedures, 127–138.https://doi.org/10.1007/978-3-031-21291-8_8
Tantry, U.S., Schror, K., Navarese, E.P., Jeong, Y.H., Kubica, J., Bliden, K.P. and Gurbel, P.A. 2021. Aspirin as an adjunctive pharmacologic therapy option for COVID-19: Anti inflammatory, antithrombotic, and antiviral effects all in one agent. Journal of Experimental Pharmacology, 13, 957. https://doi.org/10.2147/JEP.S330776
Ter Horst, S., Conceição-Neto, N., Neyts, J. and Rocha-Pereira, J. 2019. Structural and functional similarities in bunyaviruses: Perspectives for pan-bunya antivirals. Reviews in Medical Virology, 29(3), e2039. https://doi.org/10.1002/RMV.2039
Vázquez, C., Encalada, R., Jiménez-Galicia, I., Gómez-Escobedo, R., Rivera, G., Nogueda-Torres, B. and Saavedra, E. 2024. Repurposing the antidiabetic drugs glyburide, gliquidone, and glipizide in combination with benznidazole for Trypanosoma cruzi infection. Pharmaceuticals (Basel, Switzerland), 18(1). https://doi.org/10.3390/PH18010021
Veljkovic, V., Glisic, S., Muller, C.P., Scotch, M., Branch, D.R., Perovic, V.R., Sencanski, M., Veljkovic, N. and Colombatti, A. 2015. In silico analysis suggests interaction between Ebola virus and the extracellular matrix. Frontiers in Microbiology, 6(FEB). https://doi.org/10.3389/FMICB.2015.00135
Veljkovic, V., Goeijenbier, M., Glisic, S., Veljkovic, N., Perovic, V.R., Sencanski, M., Branch, D.R. and Paessler, S. 2015. In silico analysis suggests repurposing of ibuprofen for prevention and treatment of EBOLA virus disease. F1000Research, 4, 104. https://doi.org/10.12688/F1000RESEARCH.6436.1
Wong, M.W., Yi, C.H., Liu, T.T., Lei, W.Y., Hung, J.S., Liu, C.Z. and Chen, C.L. 2021. Effects of phosphodiesterase-5 inhibitor sildenafil on esophageal secondary peristalsis: Studies with high-resolution manometry. Journal of Gastroenterology and Hepatology, 36(2), 430–435. https://doi.org/10.1111/JGH.15170
Xia, Y., Sun, M., Huang, H. and Jin, W.L. 2024. Drug repurposing for cancer therapy. Signal Transduction and Targeted Therapy, 9(1). https://doi.org/10.1038/S41392-024-01808-1
Zhen, J., Zhang, C., Huang, T., Xie, L., Yan, Y., Yan, S., Zhang, J., Huang, H. and Xie, J. 2024. Drug repurposing: An antidiabetic drug Ipragliflozin as Mycobacterium tuberculosis sirtuin-like protein inhibitor that synergizes with anti-tuberculosis drug isoniazid. International Journal of Biological Macromolecules, 282, 137003. https://doi.org/10.1016/J.IJBIOMAC.2024.137003
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2025

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-CompartirIgual 4.0.
La revista Biotecnia se encuentra bajo la licencia Atribución-NoComercial-CompartirIgual 4.0 Internacional (CC BY-NC-SA 4.0)








_(2).jpg)